ADHD
A general resource page on ADHD in children and adolescents.
Attention deficit hyperactivity disorder (ADHD) is the most common neurodevelopmental disorder in the world and one of the most common disorders of childhood, with a prevalence in school aged children of around 9 to 15 percent. It is more common in boys than girls (14% boys vs 6% in girls), and in 20-25% of cases it presents with psychiatric comorbidities (e.g. oppositional defiant disorder, anxiety, or depression). A diagnosis is generally made by a clinical interview of parents and kids, but it is preferable to diagnose after information is obtained from multiple settings. If not treated, there is a significant risk in terms of social functioning, school functioning, and occupational functioning.
Diagnosis
ADHD is a persistent pattern of inattention and/or hyperactivity-impulsivity that is present before the age of 12 years, interferes with functioning or development, and is present in more than one setting (e.g. at home, school or work; with relatives or friends; required or leisure activities). A person must have at least six symptoms of inattention and/or six symptoms of hyperactivity-impulsivity to be diagnosed with ADHD.
Symptoms of inattention include:
- Making frequent careless errors or overlooking details
- Difficulty sustaining attention in tasks/activities
- Failing to complete tasks/work
- Difficulty organizing tasks
- Becoming easily distracted
- Being forgetful in daily activities
- Frequently losing important/necessary items
- Avoiding tasks that require sustained mental effort.
Symptoms of hyperactivity-impulsivity include:
- High levels of fidgeting
- Feeling restless
- Inability to stay in seat when expected
- Running or climbing at inappropriate times/places
- Talking excessively
- Blurting out answers
- Unable to wait turn
- Frequently interrupting/intrusive with others.
Widely available scales (see below) are an effective way of obtaining this information from collateral sources. It is necessary during the diagnosis process to also consider medical, psychosocial and developmental issues that could be mistaken for ADHD. It is also very important to obtain family history as it is an extremely heritable disorder. 20-25% of cases have psychiatric comorbidities (e.g. oppositional defiant disorder, anxiety, or depression).
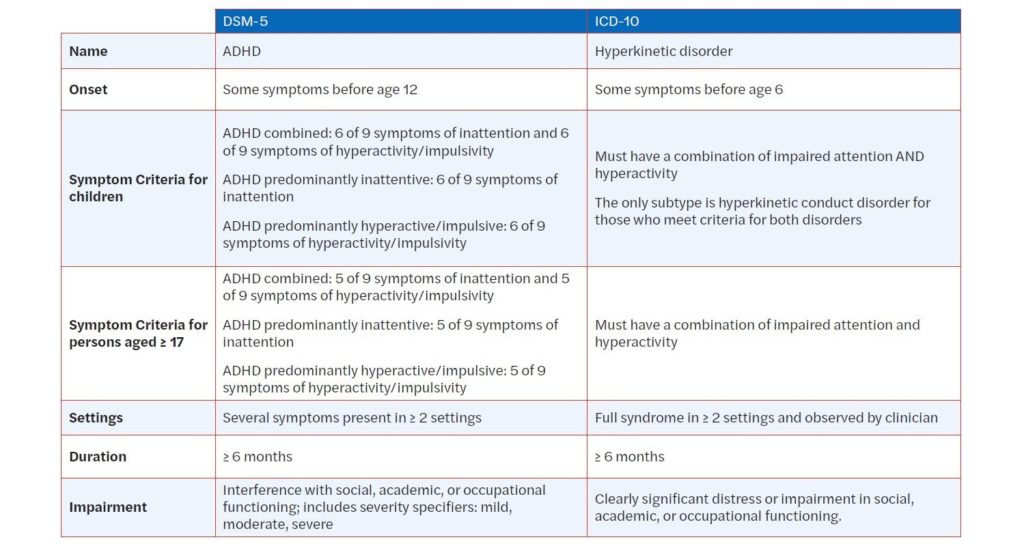
Comparison of DSM-5 and ICD-10 Diagnostic Criteria for ADHD
The table below is excerpted from “Are We Overdiagnosing and Overtreating ADHD?” Click to download a printable PDF of the table.
Rating Scales
- Vanderbilt Assessment Scales
- ADHD Rating Scale-IV – Checklists, Norms, and Clinical Interpretations
- Swanson, Nolan, and Pelham (SNAP-IV)
(Click to download a printable PDF with more detail on these Ratings Scales)
Resources for Providers
- Texas Children’s Health Toolkit
- American Academy of Pediatrics ADHD toolkit
- Clinical Practice Guideline
- JCCAP summary article on evidence-based psychosocial treatments for children and adolescents with AD/HD
- American Academy of Child and Adolescent Psychiatry ADHD Resource Center
- American Professional Society for ADHD and Related Disorders
- ADHD Clinical Pearls (MCPAP)
- ADHD Medication Visual Guide
- ADHD Medication Guide and Algorithm (see pages 15-16 for doses/ formulations)
- Comprehensive Care Pathway for ADHD: The AAP Algorithm
- Webinar on Updated AAP Guidelines (Nov 2019)
- How to Optimize Stimulant Medication for ADHD
Resources for Parents, Adolescents, and Children
- Facts for Families
- CHADD’s review of AD/HD and COVID-19
- Parent training in behavior management for AD/HD
- Strategies to support children with AD/HD at home or in the community
- Free online course for evidence-based parent management training
- National Alliance on Mental Illness
- National Attention Deficit Disorder Association